What is the process of applying for Medicare and Medicaid if you already receive disability benefits?
Senior Healthcare Advisors
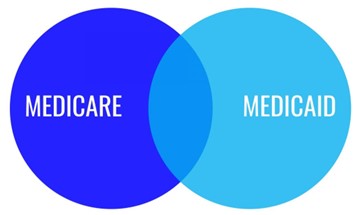
What is Medicaid? Medicaid offers healthcare coverage to low-income and disabled citizens of the United States. Each state determines the coverage details, but every state has to offer certain services, including hospital services and specific doctors.
You can also get coverage from both Medicaid and Medicare. If you meet the qualifications, Medicaid can help you pay for your Medicare coinsurance, deductibles, and/or premiums.
According to the Centers for Medicare & Medicaid Services (2022) (CMS), you should still apply for Medicaid even if you are unsure you qualify.[1] Even if you get rejected from the program, it is better than not applying. You should keep your chin up and apply the next year. Each year your eligibility can vary, so if you were denied once, you might qualify the next time.
Steps for applying for Medicare
Step One:
Check with your State Medicaid services if you are eligible.
- Call your State Medicaid office
- Review the website (Each state’s Medicaid application process and programs vary.
Step Two:
You will receive all the important information on filling out the Medicaid application. The most common reason for being denied by Medicaid is incomplete information. You must provide the necessary information before submitting your Medicaid application.
Necessary documentation
- Proof of your disability. If you know your disability will qualify you for Medicaid, your application must include the proof. For example, doctors’ notes, chiropractor information, X-rays, etc.
- Proof of your residence. You will need to include receipts for your mortgage or rent and landlord statements, which should also prove your most recent mailing address. Sending copies is recommended.
- Proof of your income, resources, and assets. Your application for Medicaid must include financial resources and bank statements.
- Proof of United States citizenship or alien status.
- Proof of other sources of income. These can include pay stubs, Veteran’s benefits, tax returns, Supplemental Security Income, retirement accounts, Social Security, and all other received income.
- A copy of your birth certificate or some evidence of your age, such as your driver’s license.
- Proof of any other insurance. You can provide your red, white, and blue Medicare card or other insurance ID card. *** Verify with your State Medicaid office to see if you need additional documentation.
Step Three:
Submit your Medicaid application. When applying for Medicaid, you must strictly follow the state’s instructions. Here are some options:
- You can visit your local Medicaid office and fill out your application in person.
- You can fill out your Medicaid application online.
***The state has up to 45 days to respond to your application and 90 days to respond to disability applications.

Application Denial:
If your Medicaid application is denied, you may want to consider appealing the decision. To do this successfully, it is essential to provide the Medicaid office with all relevant documentation and records supporting your coverage eligibility.
Suppose your application was denied due to missing information or other missing details. In that case, you should carefully review your denial record and take the necessary steps to correct any errors. This may involve gathering additional documentation or contacting the Medicaid office for guidance on how to proceed.
Regardless of why your application is denied, you must understand your rights and options when it comes to appealing this decision. You may want to consult with an experienced legal professional or advocate who can help you navigate the process and ensure that your voice is heard. With the right support, you can successfully appeal a Medicaid denial and gain access to the health care coverage you need.
Every year you must renew your application for Medicaid. To stay in the program, you must renew by submitting a new application. It gets easier each year because you will be much more familiar with the process. Things change in everyone’s life, especially their age, alien status (if you’re a legal alien), and income. So, think of it as updating the office.
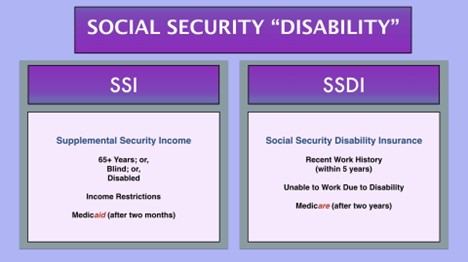
After the first 24 months of eligibility for Social Security Disability Insurance (SSDI), you become eligible for Medicare. This is referred to as the “waiting period.”
According to the Center for Medicare Advocacy (2010), “Medicare covers services that are needed to attain or maintain functioning and so can be used to prevent or postpone the loss of physical and mental capabilities”.[3]
If you have been receiving SSDI checks for two years (25 months), you will automatically be enrolled for Medicare at the beginning of your 25th month without contacting anyone.
You will get your red, white, and blue Medicare insurance card three months before starting your coverage. You will also receive a pamphlet containing all of the information about Medicare. Your card proves that you enrolled automatically in Medicare Parts A and B.
If you receive retirement benefits from Social Security, your insurance card and pamphlet will come from the Social Security Administration (SSA). If you get railroad disability annuity checks, your information packet and card will come from the Railroad Retirement Board.
Your monthly Part B premium is automatically deducted from your railroad disability annuity check or your Social Security check starting the month your coverage begins.
Unless you or your spouse has job-based insurance, you should not turn down Medicare Part B. If you do turn it down, you may end up with a premium penalty if you want to enroll for Medicare in the future.
Furthermore, your job-based coverage pays secondary to Medicare. You should consider enrolling in Medicare so you have primary coverage and, therefore, will pay less for your services.
Social Security Disability Insurance (SSDI) & Medicare coverage
You can be in the 2-year waiting period before receiving Social Security Disability Income (SSDI), or you may already be on SSDI and enrolled in Medicare. You have options either way
Social Security Disability Income (SSDI) and Medicare are two different things. SSDI is a government program that can give you financial help if you cannot work because of a medical condition. You do not need to buy health insurance through the Marketplace or anywhere else to get SSDI benefits, but people who don’t have coverage may have to pay.
Supplemental Security Income (SSI) Disability & Medicaid coverage
***If you have Supplemental Security Income (SSI) Disability, you may get Medicaid coverage automatically, or you may have to apply.***
If you get Supplemental Security Income (SSI) Disability and have Medicaid, you’re covered under the health care law.
Suppose you get Supplemental Security Income (SSI) Disability and Don’t have Medicaid
- You do not need to apply for Medicaid. SSI recipients qualify automatically for Medicaid in most states.
- In some states, you are guaranteed SSI disability, but you must enroll for it.
- In a few states, SSI doesn’t guarantee Medicaid eligibility. But most people who get SSI are still eligible.
Conclusion:
To avoid delays, always refer to your local or state Medicaid / Medicare office for the most updated information, policies and procedures.
Click here to find the Medicaid office in your state:
https://www.medicaid.gov/about-us/beneficiary-resources/index.html.
How we help
If you’re looking for the best Medicare Advantage plan that meets your needs and or have had a disability for over 24 months, we can look into plans that will enhance your Medicaid and or Disability plan. Contact our team at 888.809.1463. We have years of experience working with some of the top healthcare providers in the industry, and we can help you find a plan with options and benefits that meets your needs. Call us today at 888.809.1463.

